For the Chagas scientific community, it is urgent to establish a new and complete patient registry for the millions of people who live in vulnerable social conditions and are infected.
Based on the cancer registries in the United States and Europe, it can be observed how patient follow-up plays an important role in improving the results of prevention and treatment of patients. According to the United States CDC, this "enables researchers, clinicians, policy makers, public health professionals, and members of the public to monitor the burden of cancer, evaluate the success of programs, and identify additional needs for cancer prevention. and enforcement efforts at the national, state, and local levels. "
Along these lines, we can see that there is also a justification for establishing a registry of certain neglected tropical diseases (NTDs). Many NTDs are chronic, debilitating conditions that resemble noncommunicable diseases or chronic infections such as HIV-AIDS. Several NTDs also have uncertain treatment outcomes, while in many cases, large patient populations lack access to interventions because they are disproportionately composed of people living in extreme poverty or underserved indigenous populations. For these reasons, some ETDs may also be suitable for a registry.
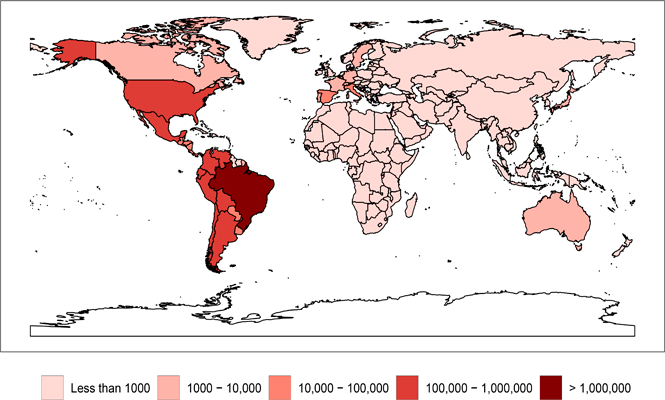
The objective of this article is to prove the urgency of establishing a registry of the 6 to 7 million people living with Chagas disease. After infection through a triatomine (bed bug) bite, oral ingestion, or vertical or blood transfusion, the protozoan parasite Trypanosoma cruzi can cause acute Chagas disease. However, this initial phase of infection is often undetected and follows a latency period that can last for years or even decades, a condition known as the indeterminate phase. Very little is known about progression. Most patients never progress to symptoms, but up to one third may enter the determined phase and develop Chagasic heart disease, also known as chronic Chagasic cardiomyopathy (CCC), and / or severe Chagasic gastrointestinal disease characterized by megacolon and / or megaesophaus. Less than 1% to 2% of patients have access to etiological treatment and, when performed in the chronic phase, there is no definitive understanding or demonstration of its long-term impact.
You can read the full article here: https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0008418
A new patient registry for Chagas disease
For the Chagas scientific community, it is urgent to establish a new and complete patient registry for the millions of people who live in vulnerable social conditions and are infected.
12 October 2020